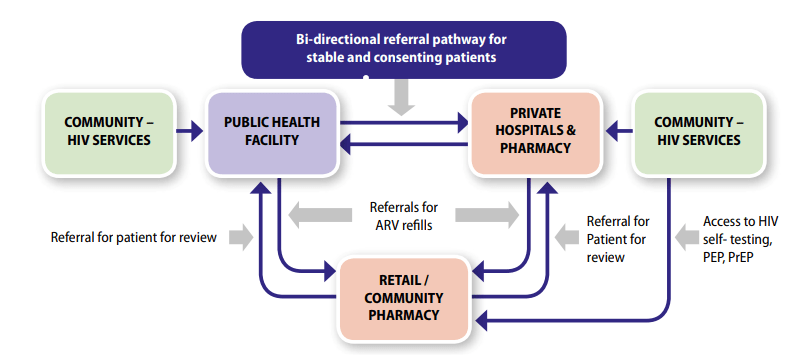
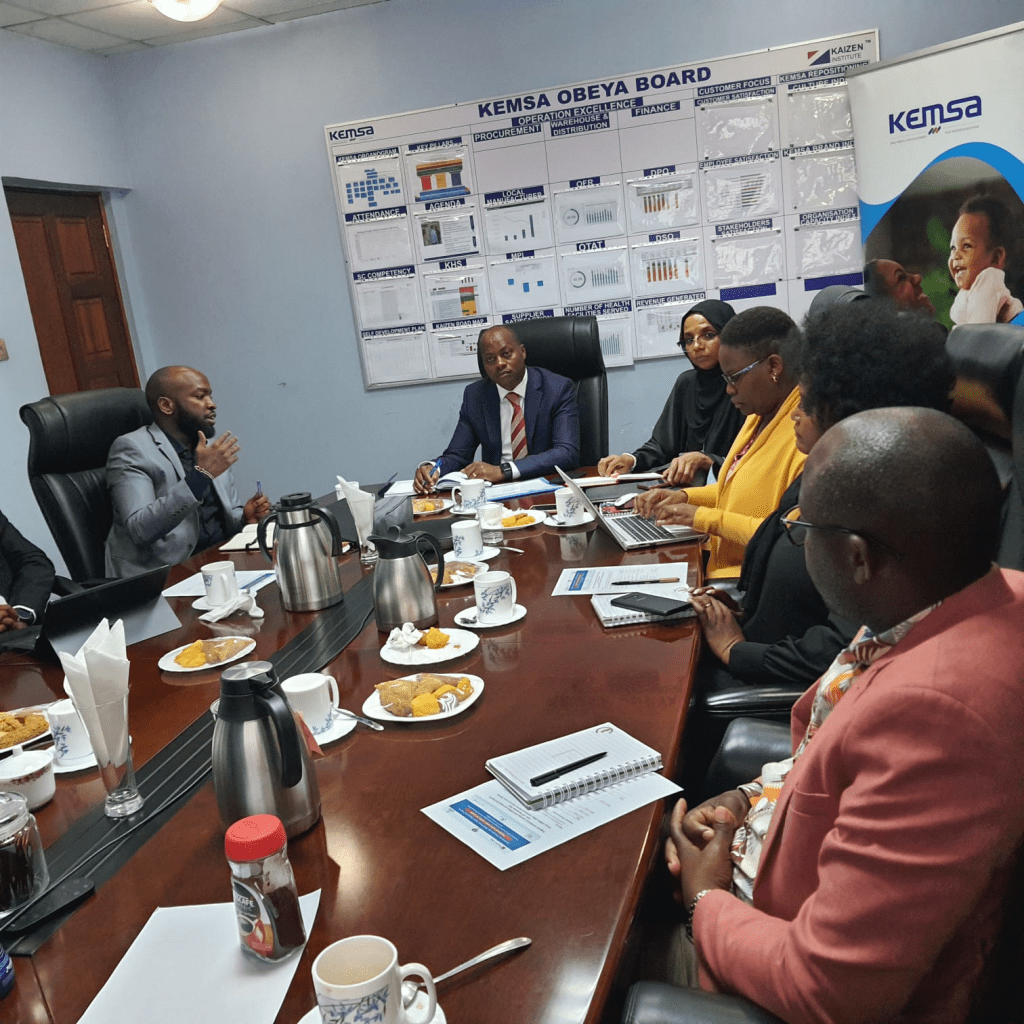
Leveraging the Private Sector to Expand Access to HIV Services in Kenya
World AIDS Day (WAD) is commemorated each year on the 1st of December. The theme for WAD 2023 is ‘Let Communities Lead’. This theme highlights the pivotal role communities have had in shaping the HIV response, as well as global health at large. Approximately 38.4 Million people are living with HIV globally. In Kenya, this …
Leveraging the Private Sector to Expand Access to HIV Services in Kenya Read More »